The Hidden Risks of Delayed Radiation Dose Feedback in Hospitals
Written by
Chris Passmore, CHP
President of Radiation Detection Company
Last Updated: June 4, 2025
In high-exposure environments like the cardiac catheterization (cath) lab, visibility into occupational radiation dose isn’t just about regulatory compliance – it’s about protecting the health and safety of clinicians who perform lifesaving procedures daily. Yet for many, timely radiation dose feedback is elusive, and the consequences are quietly accumulating.
The Reality of Radiation Exposure in Modern Hospitals
Interventional cardiologists and staff in cath labs face repeated exposure to ionizing radiation from procedures like:
- Diagnostic cardiac catheterizations
- Percutaneous coronary interventions (PCI)
- Complex chronic total occlusions (CTO)
- Transcatheter aortic valve replacements (TAVR)
These procedures are often lengthy and involve significant fluoroscopy time, increasing cumulative dose risk.
The Data Void: How Passive Dosimeters Can Leave Clinicians Unprotected
Despite these risks, many hospitals still rely on passive dosimetry, such as optically stimulated luminescence (OSL) or thermoluminescent dosimeters (TLD), to monitor exposure.
While passive dosimetry can be a great option in lower-risk environments, they're not always ideal for workers in high-exposure environments.
Here's why: passive dosimeters deliver radiation dose information only after the end of the wear cycle (typically 30 days), with a delay of up to 45 days before results are available. During that time, clinicians continue to work, unaware of their actual exposure levels. That’s 45 days of work and radiation exposure without dose feedback on the first 30 days. I call this the Passive Dosimeter Data Void.
A 45-Day Simulation: Radiation Dose Accumulation in a High-Exposure Environment
I modeled a 45-day dose simulation for an interventional cardiologist at a large hospital to further illustrate the data void: the simulation incorporated real-world scheduling patterns, average procedure times, and typical dose ranges.
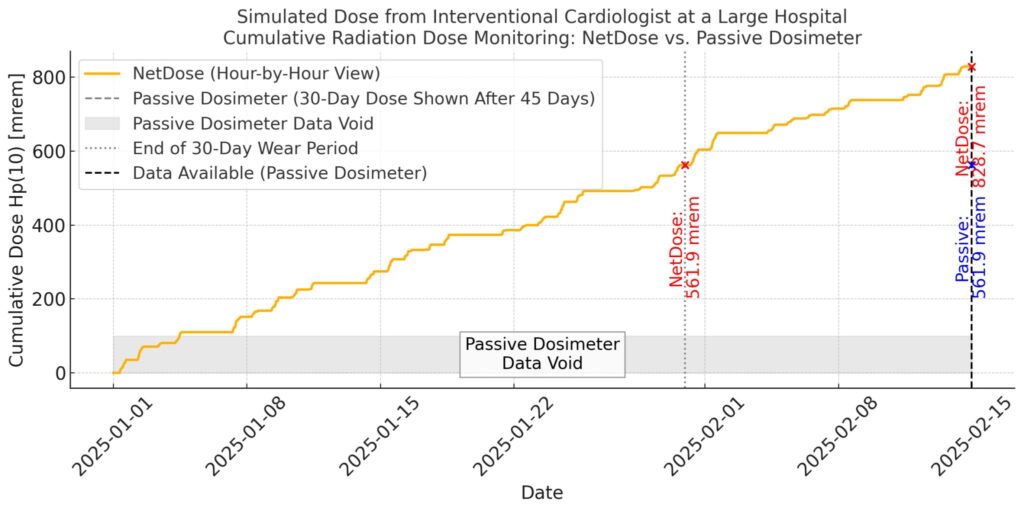
The difference in visibility is stark:
- With passive dosimetry, we see a flat line that is silent during the wear period and only jumps at the end of the month.
- With the NetDose™ digital dosimeter, we see an immediate and continuous curve, reflecting real-time accumulation, updated as procedures occur.
The results were eye-opening:
- By Day 30: The simulated Hp(10), or deep dose equivalent, reached 562 mrem (5.62 mSv).
- By Day 45: That number climbed to 829 mrem (8.29 mSv).
These are significant exposures, and they occurred without the worker having any real-time feedback on dose accumulation.
Delayed dose data puts workers in high-exposure environments at risk without even knowing it.
How Real-Time Dose Monitoring Improves Safety and Compliance
While other digital dosimetry options exist, few offer the dose resolution and temporal granularity needed in fast-paced clinical settings. Enter NetDose™: a digital dosimeter that offers hour-by-hour, case-by-case dose visibility.
With NetDose™, workers no longer wait weeks for feedback. Instead, they can:
- Monitor radiation exposure throughout the day
- Review case-specific dose metrics
- Make proactive adjustments to minimize exposure
- Identify high-risk patterns or outliers quickly
This level of insight empowers radiation safety officers (RSOs), imaging directors, and frontline clinicians to make informed decisions in near real-time, not weeks later.
Know Your Radiation Dose, Know Your Risk
The future of radiation safety in high-risk clinical environments lies in data transparency and timely feedback.
Passive dosimetry serves its purpose in lower-risk settings, while digital dosimetry shines in high-risk environments. Different offerings allow organizations to be selective and choose the most appropriate dosimetry monitoring solution for each unique environment and role.
NetDose™ offers more visibility for employees once caught in the data void. When hospital employees know their dose, they know their risk – and they can take corrective actions to avoid radiation safety and compliance issues.
Contact RDC Today
Want to learn more about digital dosimetry from Radiation Detection Company? Get answers to all of your NetDose™ questions, and learn how down-to-hourly reporting can benefit your organization.
Get a quote or contact us today to get started.



