
Dosimeter badge services for medical, dental, and veterinary businesses
Learn how Radiation Detection Company’s easy-to-use dosimetry solutions can boost the efficiency of your practice.

Written by
Chris Passmore, CHP
President of Radiation Detection Company
Last Updated: October 20, 2025
Webster calculations provide a practical way to accurately estimate effective dose equivalent (EDE) when lead aprons create non-uniform radiation fields. For medical physicists, Radiation Safety Officers (RSOs), and healthcare leaders, understanding these formulas is essential to compliance, safety, and clarity in dosimetry programs.
Lead aprons reduce dose. Unfortunately, they don’t reduce the confusion around Webster calculations (also known as EDE1, EDE2, Webster 1, and/or Webster 2).
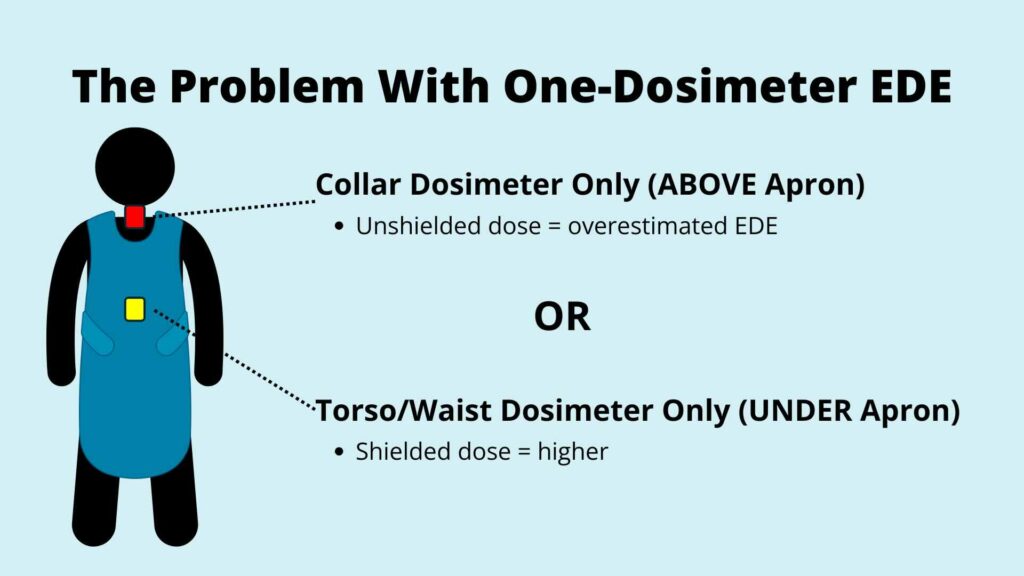
In interventional radiology, cardiology, and fluoroscopy suites, personal protective equipment (PPE) like lead aprons, protect staff from scatter or direct beam fluoroscopic X-ray radiation fields. But because the apron shields only part of the body, a single dosimeter reading doesn’t reflect actual whole body exposure.
Some facilities try to record the highest measured dose as the whole body exposure, but that method typically overestimates the actual dose, leading to overestimated reports and unnecessary concerns.
That’s where Webster calculations come in. These equations combine dosimeter readings to estimate a more realistic EDE, ensuring accurate dose tracking and regulatory compliance.
The problem? Different vendors use different shorthand (EDE1, EDE2, Webster 1, Webster 2), leaving facilities wondering which formula is in play. The result is unnecessary confusion, audit challenges, and inconsistent reporting.
This guide unpacks Webster calculations, explains why they matter, and shows how to apply them clearly in your dosimetry program.
Need to come back to this resource when you have more time? Get the free download here: Webster Calculations Guide.
When a worker wears a lead apron, the dosimeter under the apron records a much lower dose than unshielded areas like the head, neck, or arms, creating a non-uniform radiation field that complicates accurate dose assessment.
In 1989, E.W. Webster proposed a practical solution: methods that combine the deep dose equivalent, Hp(10), from one or two dosimeters and take credit for the shielding provided by the lead apron, producing a more realistic estimate of EDE – the dose that correlates to whole body risk. Webster’s mathematical solution remains the foundation of occupational radiation monitoring today.
Learn more about radiation safety fundamentals with this resource – Ultimate Radiation Badge Guide: Everything You Need to Know About Dosimetry Badges.
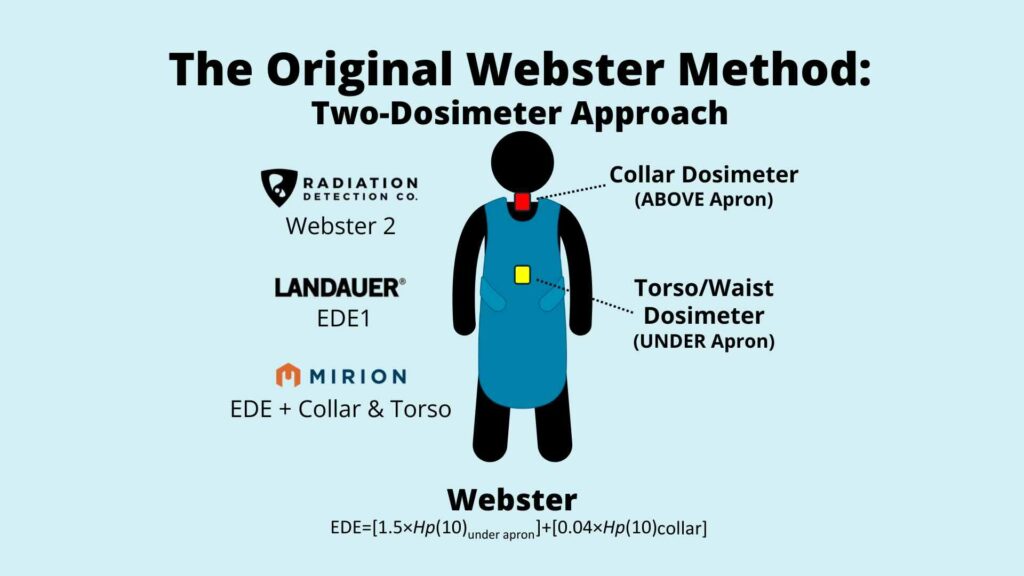
Webster’s first method assumed the worker was wearing two dosimeters: one under the apron at the torso or waist and one at the collar.
This method is best suited for staff exposed to continuous or prolonged fluoroscopy.
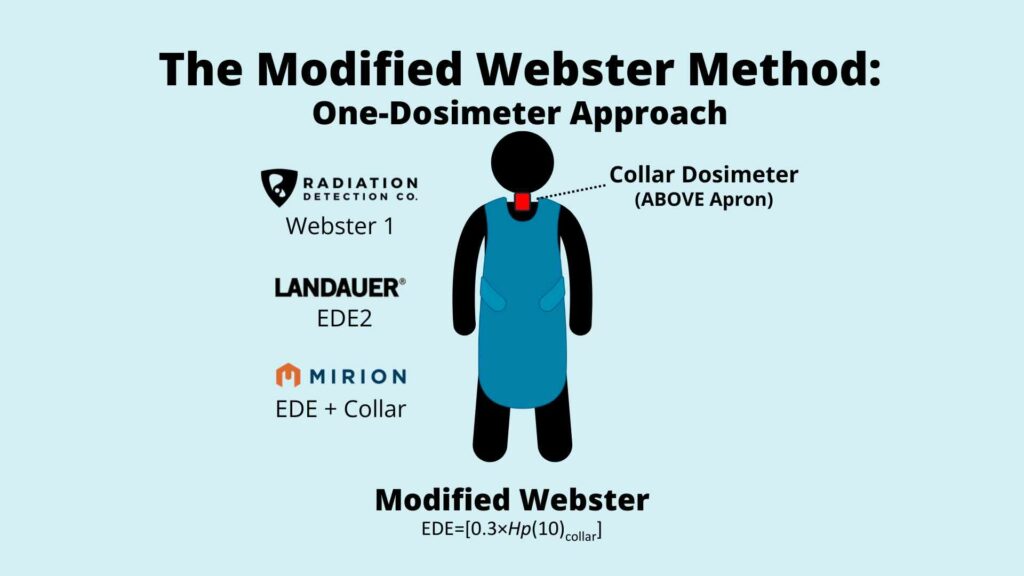
Later came the modified method for the one-dosimeter scenario.
This calculation is efficient and practical.
Really, the “best” Webster calculation is one that accurately reflects the number of dosimeters used.
In short: if you’re using two dosimeters, choose the original Webster. If you’re using one dosimeter, use the modified Webster. Either way, keep it consistent and spell out exactly how many dosimeters, where they’re worn, and which Hp(10) formula is being applied to calculate the EDE.
It sounds simple enough, so why the confusion? Well, that leads me to my next point …
The challenge here isn’t the physics, it’s the terminology. The confusion began when vendors introduced their own shorthand.
Dosimetry providers have used differing verbiage to describe their preferred Webster calculations.
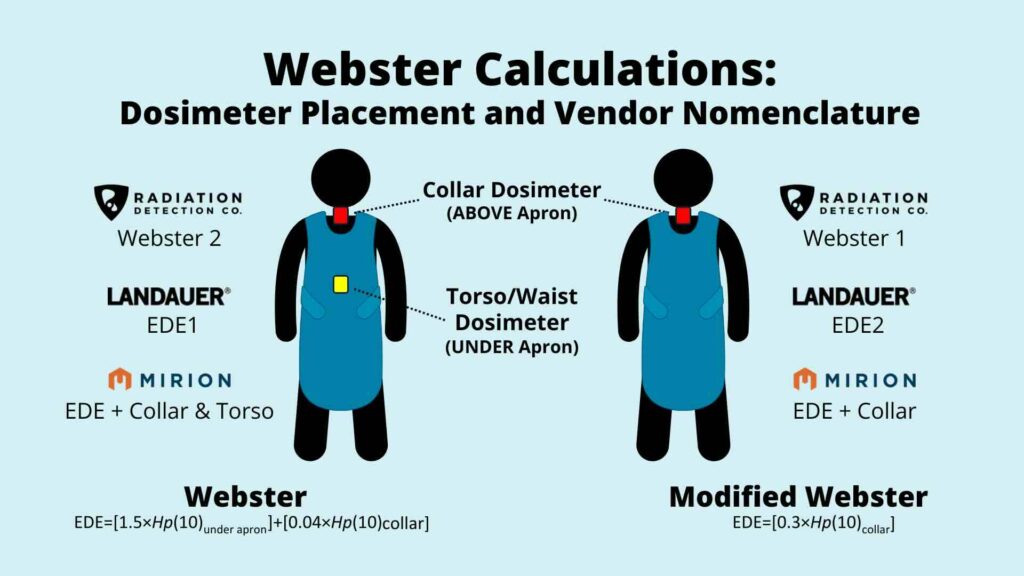
Which means that every time someone says, “We’re using EDE1,” you have to stop and ask, “Okay, but is that Landauer’s EDE1, RDC’s Webster 2, or Mirion’s EDE … and where are the dosimeter(s) located?”
So, what do the regulatory guidelines say? Well, none of the standards (NCRP 122, ANSI/HPS N13.41, or NRC/NUREG guidance) ever use the terms “EDE1” or “EDE2.” Instead, they simply present the equations.
For extra clarity, here’s some regulatory context:
Because regulatory standards never mention “EDE1” or “EDE2,” relying on shorthand makes audits messy. A hospital might say it’s using EDE1, but unless the placement and formula are spelled out, auditors can’t tell if that means Landauer’s, RDC’s, or Mirion’s reporting method.
While regulators recognize the validity of Webster calculations, they may need to be reminded which calculation is being used. Audit clarity depends on documenting exactly how EDE is calculated.
Bottom line: Webster shorthand causes ambiguity. If you want to avoid audit-induced headaches, be explicit: always spell out the number of dosimeters, placement(s), and the equation used to calculate EDE.
The type of Webster calculation you apply depends on the placement and number of dosimeters used. Each clinical environment presents a unique challenge: balancing accurate dose assessment with workflow practicality.
Learn more about why compliance matters and how to design a cost-effective program that keeps your team safe while meeting federal, state, and industry-specific requirements with this resource – Complete Dosimetry Program Management Guide: Setup, Compliance & Cost Optimization.
Here’s how Webster methods play out across common settings.
Fluoroscopy is the reason Webster calculations exist (Niklason, Marx, & Chan, 1995). These environments expose workers to prolonged scatter radiation from continuous X-ray use during guided procedures. Interventional radiologists, technologists, and nurses often stand close to the beam for extended periods.
The number of dosimeters used in high-dose fluoroscopy settings depends on state regulations.
If you have a choice, a two-dosimeter Webster approach (collar + under the apron at the waist) is the gold standard. The under-apron dosimeter captures the shielded portion of the body, while the collar dosimeter measures exposure to unshielded regions such as the thyroid, head, neck, and upper arms. Combining both readings via the original Webster equation gives a realistic EDE that satisfies NRC and NCRP recommendations.
Still, the modified Webster is safe to use in some states, which requires just a single dosimeter at the collar.
Failing to follow state guidance and properly document the number and placement of dosimeters can result in inaccurate reporting and put your compliance at risk.
Bottom line: In fluoroscopy, precision matters – use the method that follows state regulations and document which equation you’re applying.
In surgical settings, fluoroscopy is often intermittent, used for positioning or verification rather than continuous imaging. Surgeons, anesthesiologists, and nurses may wear lead aprons for protection but experience brief, intermittent exposures.
Again, the number of required dosimeters will depend on state regulations. However, if you have a choice, there are pros and cons to using each method in the operating room.
The collar-only (modified Webster) approach is easier to place in the correct location consistently. Modified Webster is both efficient and sufficient, provided staff exposure is verified to remain low.
On the other hand, two dosimeters provide a more accurate assessment.
To maintain compliance, facilities should note which Webster method is being used along with justification based on low exposure frequency and dose rates. Regular program reviews help ensure the assumption remains valid as procedure volumes or imaging practices change.
Bottom line: In operating rooms, staff should use the method that follows state regulations and provide justification for the number of dosimeters used.
Dental offices, veterinary practices, and orthopedic clinics represent low-dose, low-frequency radiation environments. Scatter radiation from fixed or handheld X-ray units is generally minimal, and most exposures are brief.
Depending on the state regulations, some staff may be required to wear lead aprons, which may necessitate the use of a two-dosimeter Webster calculation.
In states with more flexibility, the modified Webster calculation (one collar dosimeter) can strike the right balance between practicality and protection, simplifying compliance without overburdening small teams or inflating costs.
That said, consistency is key: workers should wear dosimeters during every radiographic procedure with proper placement to ensure accurate readings. Program consistency and traceable documentation are essential.
Bottom line: Follow state guidelines with considerations for lead aprons, stay consistent, and document accordingly.
Cardiology labs are among the most scrutinized areas for radiation dose compliance because staff routinely perform complex, long-duration procedures involving continuous fluoroscopy.
These labs typically involve cardiologists, nurses, and technologists who work close to high-scatter regions for hours at a time. As a result, regulators and auditors often focus on whether the reported doses truly represent whole body exposure.
Again, the best recommendation is to follow state guidance. A consistent and thoroughly documented Webster method provides the clearest compliance path. It helps facilities meet state and NRC regulations and creates transparency and confidence for radiation safety committees.
Bottom line: Cardiology labs can stay audit-ready with a proactive radiation safety program. Follow state and NRC guidelines, practice consistent adherence, and provide clear documentation.
The two-dosimeter Webster method can protect staff by offering an additional layer of precision in documentation, especially when paired with digital dosimetry systems like NetDose™.
If a dose report trends high unexpectedly, having down-to-the-hour detailed Webster documentation allows teams to quickly identify whether the issue is procedural, shielding-related, or purely operational.
Bottom line: Digital dosimetry offers an added layer of radiation safety and proactive compliance.
Webster calculations are essential tools for modern dosimetry. They account for apron shielding, align reported doses with regulatory expectations, and reduce compliance risks by providing a layer of specificity required for dose reports. The formulas are straightforward – it’s the vendor shorthand that creates confusion. Choose the dosimeter placement and EDE calculation that works for your organization, stick with it, and document accordingly to stay safe and compliant.
Webster calculation clarity is an essential component of an efficient dosimetry program. By spelling out dosimeter count, placement, and formula, facilities can ensure clear reporting, pass audits confidently, and keep workers safe without unnecessary complexity.
Radiation Detection Company simplifies Webster calculation reporting through precise dosimeter calibration, clear vendor terminology, and expert support, helping over 40,000 organizations maintain confidence in their compliance and safety data.
Take the guesswork out of dosimetry. Contact RDC today to see how we can help you enhance your radiation safety program.
Webster calculations are formulas that adjust dosimeter readings to estimate effective dose equivalent (EDE) when workers wear lead aprons. There are two Webster calculations:
Aprons create non-uniform radiation fields. Webster formulas balance shielded and unshielded measurements to give a realistic whole body dose for accurate dose reports.
Radiation Detection Company uses Webster 1 and Webster 2 to describe the original Webster and modified Webster calculations, respectively.
Yes, regulatory guidelines acknowledge the use of Webster calculations and avoid shorthand terms – compliance depends on clear documentation of the method used. However, you should consult your state’s regulations to ensure compliance.
No. They supplement dosimeter readings by correcting for shielding effects. The raw data still comes from dosimeters; regulatory agencies require consistent dosimeter use.

Learn how Radiation Detection Company’s easy-to-use dosimetry solutions can boost the efficiency of your practice.