
Optimizing Fetal Monitoring Programs in 2026
Written by
Gregg Daversa, RT(R)(CT)(MR)
Director of Healthcare Sales
Last Updated: January 21, 2026
An effective fetal monitoring program protects declared pregnant workers by combining disciplined monthly fetal dosimetry, clearly defined protocols, and real-time dosimetry that allow safety teams to manage exposure proactively rather than reactively.
Across healthcare organizations, I see a wide range of fetal monitoring programs. Some are well-designed and consistently executed. Others technically meet requirements but depend heavily on delayed data, informal processes, or assumptions about exposure that aren’t always accurate.
In nearly every case, the challenge isn’t awareness. Most organizations understand the importance of protecting declared pregnant workers from exceeding occupational radiation exposure during pregnancy. The gap shows up in how organizations reliably carry out fetal monitoring month after month, how they review exposure data, and how quickly the program can respond when exposure trends begin to change.
As healthcare organizations move into 2026, fetal monitoring programs are increasingly expected to provide timely visibility, documented decision-making, and proactive intervention, especially as digital tools, audit expectations, and workforce transparency continue to evolve.
A strong fetal monitoring program isn’t built around a single policy or badge. It’s built around repeatable processes that go beyond simple recordkeeping to give safety teams visibility throughout the pregnancy and give workers confidence that exposure is being actively managed.
In the sections that follow, I’ll walk through what those processes look like in practice: how to structure monthly fetal badge protocols, when and how to use alerts effectively, and where digital dosimetry can strengthen both oversight and peace of mind for declared pregnant workers.
Key Takeaways
- Monthly fetal dosimeter badge protocols provide the most reliable foundation for fetal monitoring
- Real-time dosimetry allows Radiation Safety Officers (RSOs) to respond early instead of reacting after threshold limits have been reached
- Digital dosimeters improve visibility, trend recognition, and worker reassurance
- Clear policies and consistent communication reduce common badge-related errors
- Proactive fetal monitoring reduces compliance risk, lowers worker anxiety, and supports worker confidence
Building a Strong Fetal Monitoring Program
Pregnancy Declaration and Program Structure
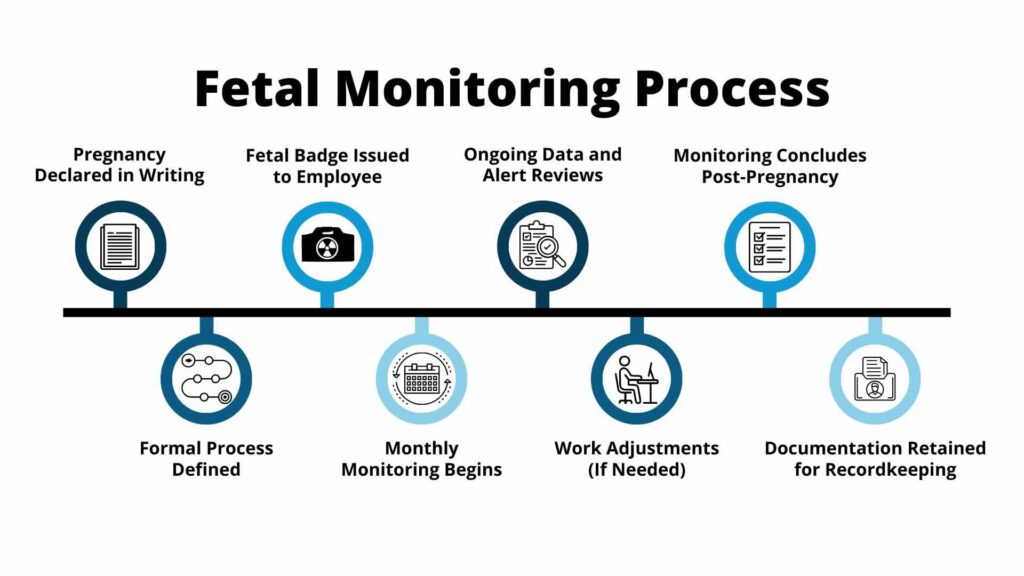
Fetal monitoring begins when a worker voluntarily declares pregnancy in writing to the RSO or management, typically including an estimated date of conception. This step is straightforward, but what follows determines whether the program functions smoothly or becomes inconsistent over time.
A voluntary declaration of pregnancy means that the employee has opted into the radiation safety program, subject to new administrative limits and a lower dose limit.
Once a written declaration is made, the organization should move immediately into a defined process. That process should clearly explain how fetal monitoring is initiated, how exposure will be reviewed, and what role the worker, RSO, and leadership each play. When policies are vague or handled informally, expectations can shift from one department to another, which introduces risk and confusion.
A well-structured policy removes ambiguity. It establishes when a fetal dosimeter badge is issued, how monitoring data is reviewed, when job duties may be adjusted, and how fetal monitoring formally concludes. It also reinforces confidentiality while ensuring that exposure data is still reviewed consistently and documented appropriately.
Is your radiation safety program looking to formalize fetal monitoring within a broader safety framework? Check out our Complete Dosimetry Program Management Guide for best practices on policy development, documentation, and program oversight.
Monthly Fetal Dosimeter Badge Protocols
Monthly fetal monitoring is the operational backbone of an effective program. Without consistent monthly data, it becomes very difficult to identify trends early enough to take meaningful action.
Once an employee declares a pregnancy, the RSO should issue a dedicated fetal dosimeter badge in addition to the standard whole body badge.
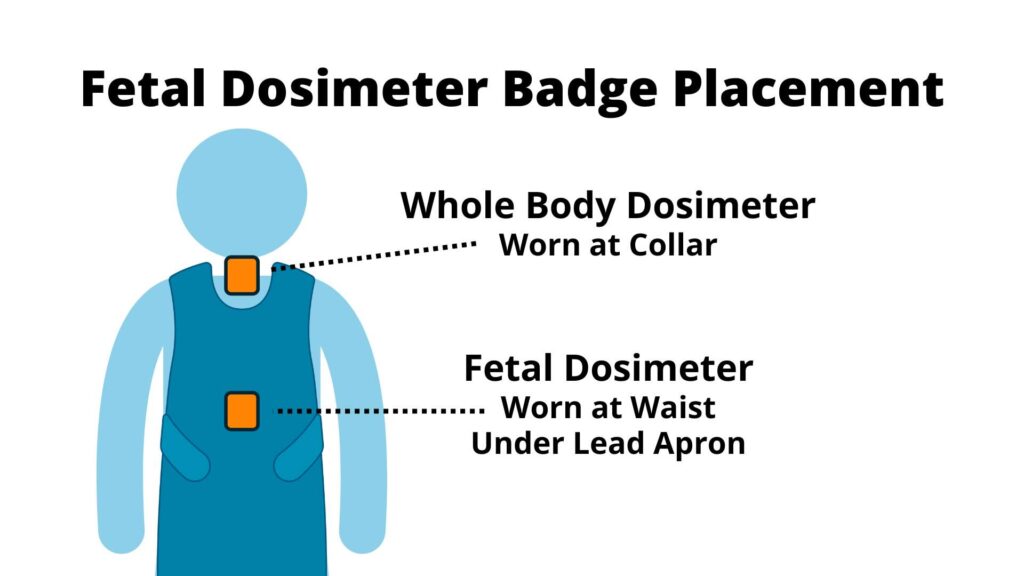
The pregnant employee should always wear the fetal dosimeter badge at waist level, underneath any lead apron or shielding devices, so that it reflects fetal exposure as accurately as possible. This placement detail seems simple, but it is one of the most common sources of error when programs are not reinforced through training and reminders.
Correct badge placement is critical for accurate fetal dose measurement. Get practical guidance on proper wear, common mistakes, and compliance reminders with our free resource: Radiation Badge Wearing Tips.
Equally important is the exchange and review frequency. Organizations should exchange fetal dosimeter badges and return the badges to the dosimetry provider each month without exception, even if the organization uses a different cycle for whole body dosimeters.
Federal regulations specify a limit of 500 mrem for the entire gestation period, much lower than the annual limit, and a monthly limit of 50 mrem.
Monthly intervals create manageable checkpoints and adhere to federal regulations. If exposure is higher than expected in a given month, there is still time to investigate causes and make adjustments before cumulative exposure becomes a concern.
Programs that treat fetal badges as secondary or “extra” often miss these early warning signs. Consistency is what turns monitoring into management.
Known Barriers: Leaner Staffing and Higher-Exposure Assignments
One factor that has become increasingly important in recent years (and will continue to shape fetal monitoring programs in 2026 and beyond) is leaner staffing across imaging departments. With fewer technologists available to support procedure volumes, declared pregnant workers are often spending longer stretches of time assigned to higher-exposure modalities such as fluoroscopy, interventional procedures, or hybrid rooms.
In these environments, even small changes in scheduling or case mix can have a measurable impact on monthly fetal dose. What might once have been a short, shared assignment can turn into extended times in the fluoroscopy imaging or treatment rooms simply because fewer qualified staff are available to rotate in. When that happens, cumulative exposure can build more quickly than expected, even when proper shielding and technique are being applied.
This reality makes consistent monthly fetal dosimetry (and, where available, real-time dose visibility) more critical than ever. As staffing models tighten, programs can no longer rely on assumptions about exposure based on historical workloads. Instead, they need timely data to confirm whether assignments remain appropriate, identify when exposure is drifting upward, and make informed adjustments before dose limits become a concern.
Understanding how different monitoring focuses translate into insight is key to managing exposure proactively, especially when staffing and assignment flexibility are limited. Not all monitoring data serves the same purpose, and knowing what each view of exposure reveals can make the difference between simply recording dose and actively managing it.
Proactive Fetal Dosimetry
The table below illustrates how different monitoring focuses translate raw dose data into actionable insight – an increasingly important distinction as staffing constraints limit flexibility in assignment and scheduling.
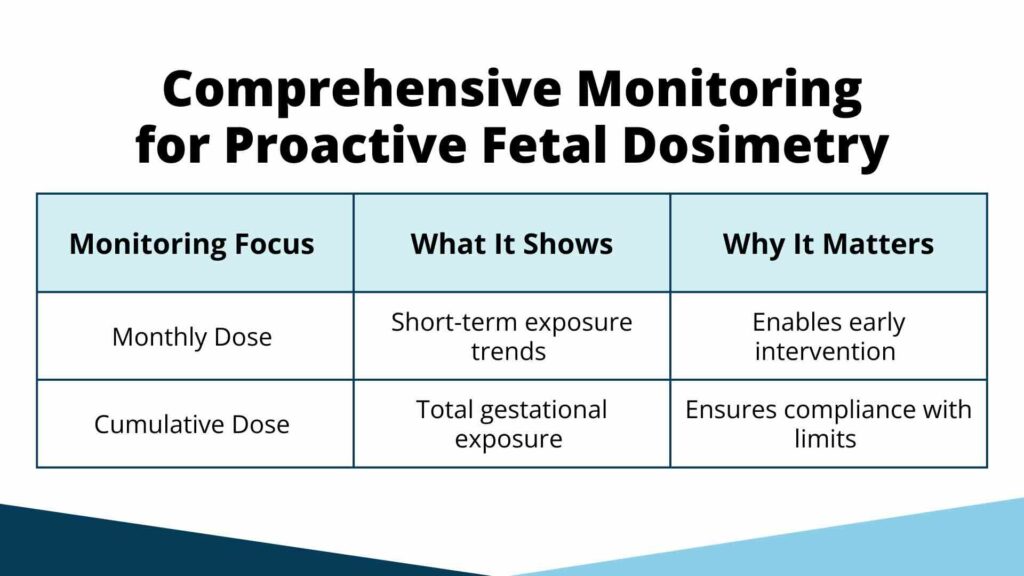
In 2026 and beyond, consistent monthly protocols matter even more as healthcare teams manage higher procedure volumes, rotating assignments, and leaner staffing models that can make informal monitoring practices harder to sustain.
Explore Fetal Monitoring Solutions
Real-Time Data and Ongoing Oversight
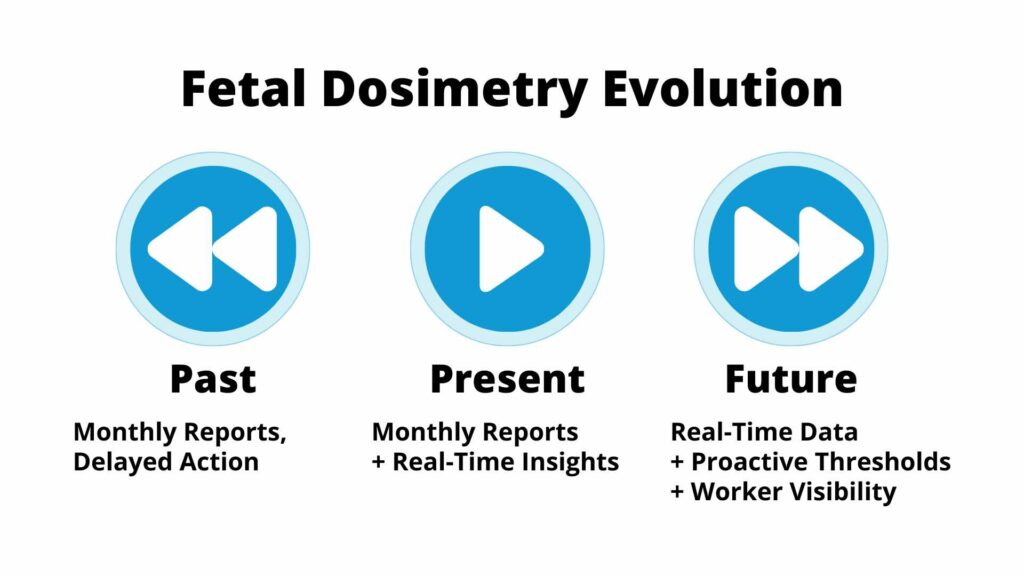
By 2026, many organizations no longer view real-time or near real-time dose visibility as an enhancement – it is increasingly seen as a baseline expectation for managing occupational and fetal exposure responsibly.
Even with monthly monitoring in place, relying on delayed or manual review of dosimetry data can create unnecessary stress and uncertainty, particularly for declared pregnant workers. Traditional dosimeter processing introduces latency between exposure and reporting, which limits an RSO’s ability to act quickly and may allow potential risks to the pregnancy or fetus to go unidentified for weeks.
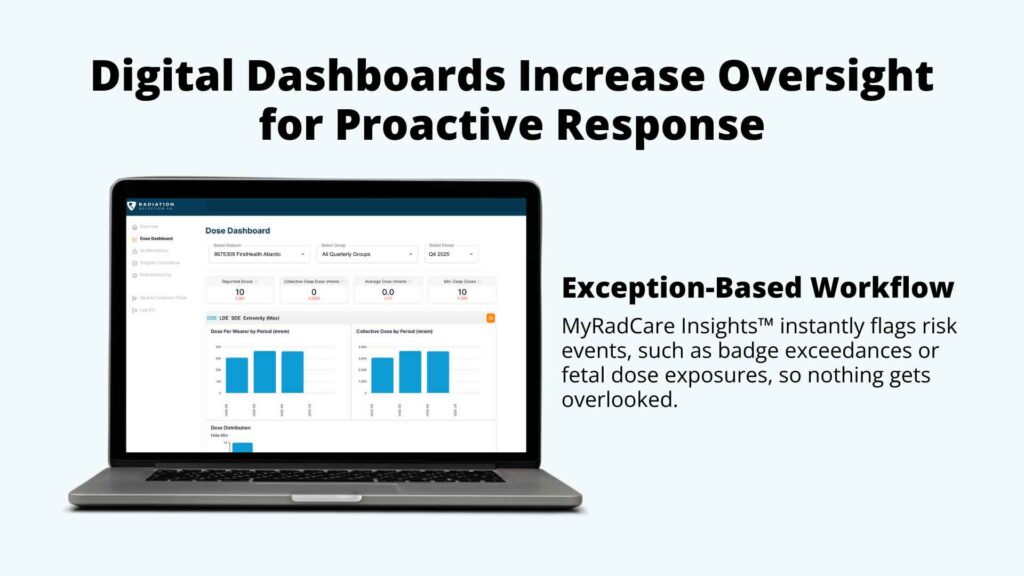
Digital dosimetry changes this dynamic by providing immediate access to cumulative and time-specific dose data. With near real-time visibility, RSOs can make timely, informed decisions such as adjusting workloads or reassigning tasks before dose trends become a concern. Automated alerts add a critical layer of protection by drawing attention to changes that might otherwise be overlooked during routine review.
Alerts can be configured to notify safety staff when doses approach predefined thresholds, when cumulative exposure trends toward gestational limits, or when an unexpected spike occurs compared to prior periods. When these alerts are shared transparently with both the declared pregnant worker and appropriate safety personnel, everyone is working from the same information at the same time, leading to calmer, more proactive conversations and faster intervention.
Dashboards that display dose trends over the course of pregnancy are especially valuable. They allow RSOs to identify gradual increases tied to workload, procedure mix, or staffing patterns: insights that are difficult or impossible to detect when relying solely on isolated monthly reports.
To explore how real-time data and AI-driven analytics support a shift from reactive review to proactive radiation safety management, read Digital Dosimetry and AI: Shifting from Reactive to Proactive Radiation Safety.
Dose Limits, ALARA, and Practical Decision-Making
In the United States, the Nuclear Regulatory Commission (NRC) sets fetal dose limits at 0.5 rem (5 mSv) for the entire pregnancy, with guidance to avoid concentrating exposure early in gestation. While these limits provide an important framework, they are only part of the picture.
ALARA remains the guiding principle in fetal monitoring, and ALARA works best when it is informed by real data. Monthly exposure trends make it possible to move beyond theoretical discussions and into practical decision-making. Instead of asking whether exposure might be high, RSOs can see when and where exposure is actually occurring and respond accordingly.
As state, NRC, Joint Commission, and DNV scrutiny increases, and audits and surveys place greater emphasis on documentation and decision rationale, programs that can demonstrate how real-time or monthly data informed ALARA decisions are better positioned to defend their practices.
This approach allows organizations to make targeted adjustments (rather than broad restrictions) while still maintaining a strong safety margin.
Managing Work Duties and Reducing Exposure
When fetal monitoring data indicates higher-than-expected exposure, the goal is not to remove the worker from their occupational responsibilities. In most cases, modest adjustments can significantly reduce exposure without disrupting operations.
Redistributing higher-dose procedures, improving shielding placement, modifying schedules, or reinforcing best practices around badge wear can all have a meaningful impact.
In lean staffing environments, these adjustments often need to be made proactively, as extended assignments in fluoroscopy or interventional settings can become the norm rather than the exception.
Training plays an important role here. Small lapses, such as wearing the fetal badge incorrectly or swapping badges, can distort data and lead to unnecessary concern or missed risk.
When radiation safety teams consistently review data on a monthly basis, these issues tend to surface early, when they are easiest to correct.
Ending Fetal Monitoring and Maintaining Records

Fetal monitoring should conclude as deliberately as it begins: when pregnancy ends due to delivery or leave, the RSO should collect the fetal badge and clearly document the termination date. Cumulative exposure records should be finalized and retained according to institutional and regulatory requirements.
Maintaining clear, complete records supports compliance and allows programs to evaluate their own effectiveness over time. Comparing fetal badge data with whole body badge data can also help confirm proper badge use and identify inconsistencies that may warrant additional training.
The Value of Digital Dosimetry in Fetal Monitoring
Traditional TLD and OSL badges remain reliable tools when used correctly, but digital dosimetry expands what fetal monitoring programs can realistically accomplish.

Digital systems reduce the delay between exposure and awareness, allowing RSOs to respond more quickly when something unexpected occurs. They also provide more frequent data points, which makes it easier to identify patterns that would otherwise remain hidden in monthly averages.
To see how real-time visibility and automated alerts are delivered in practice, explore NetDose™ digital dosimeters.
Automated alerts and centralized dashboards further strengthen oversight, while access to timely exposure data can be reassuring for declared pregnant workers. Knowing that exposure is being actively monitored (not just recorded) goes a long way toward building trust in the program.
From a program management standpoint, digital dosimetry also supports consistency, documentation, and defensibility, particularly during audits or inspections.
Learn how delayed dose reporting can limit a program’s ability to intervene early and how digital tools help close that gap: The Hidden Risks of Delayed Radiation Dose Feedback in Hospitals.
Monitoring Thresholds for Pregnant Employees
One of the challenges in fetal monitoring is that regulations typically define maximum limits, but they don’t always explain how organizations should manage exposure before those limits are reached. That gap is where proactive monitoring becomes most valuable.
Rather than treating fetal dose limits as a single number to check at the end of pregnancy, effective programs establish internal monitoring thresholds that prompt review and discussion well in advance. These thresholds are not regulatory requirements; they are management tools designed to surface trends early, support ALARA decision-making, and give safety teams time to respond thoughtfully.
The example below illustrates how a fetal monitoring program might use monthly and cumulative dose thresholds to guide oversight throughout pregnancy. The specific values used for monitoring thresholds matter and should be selected carefully based on regulatory guidance, institutional policy, and the nature of the work being performed.
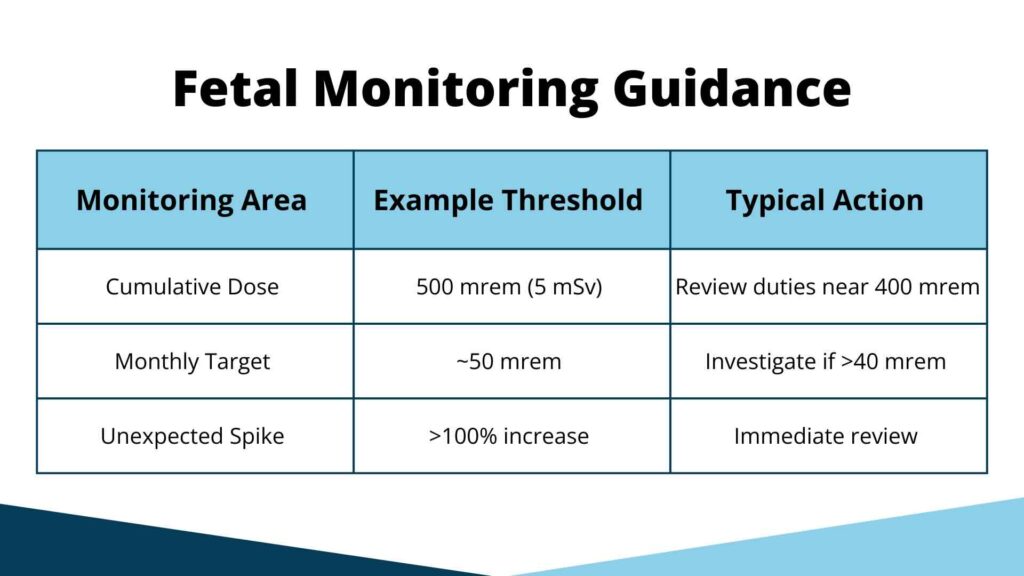
In more mature programs today, these thresholds are often embedded directly into digital monitoring platforms, allowing RSOs to move from manual review toward standardized, repeatable oversight as programs scale.
What distinguishes a proactive fetal monitoring program is how those numbers are used –by defining clear trigger points, reviewing data consistently, and acting on early indicators to adjust work practices before exposure becomes a concern.
Benefits for Workers and Organizations
When fetal monitoring programs are implemented thoughtfully and consistently, the benefits extend beyond compliance. Declared pregnant workers feel supported, confident, and informed, RSOs gain clearer oversight, and leadership avoids surprises during inspections or surveys. Over time, proactive monitoring also reduces liability risk and supports better staffing and workflow decisions.
Perhaps most importantly, these programs reinforce a culture of safety: one where exposure is managed deliberately rather than explained after the fact.
Proactive Fetal Monitoring for 2026 and Beyond
An effective fetal monitoring program is built on consistency, visibility, and clear decision points.
Monthly badge protocols, automated alerts, and digital dosimetry allow organizations to manage fetal exposure proactively while supporting declared pregnant workers with transparency and confidence.
As expectations around transparency, data access, and worker engagement continue to rise, fetal monitoring programs that rely solely on delayed reporting will increasingly feel out of step with modern radiation safety practices.
Frequently Asked Questions
What is fetal monitoring in radiation safety?
Fetal monitoring tracks radiation exposure to a declared pregnant worker’s fetus using a dedicated fetal dosimeter badge throughout pregnancy.
Where should a fetal dosimeter badge be worn?
The fetal badge should be worn at waist level, underneath any lead apron or shielding, to best reflect fetal dose.
How often should fetal dosimeters be exchanged?
Monthly exchange and review is considered best practice, regardless of the organization’s standard badge cycle.
What is the fetal dose limit during pregnancy?
In the US, guidance commonly limits fetal exposure to 500 mrem (5 mSv) over the full pregnancy, following ALARA principles.
How does digital dosimetry improve fetal monitoring?
Digital dosimetry provides faster feedback, automated alerts, clearer trend visibility, and greater confidence for both workers and safety teams.
Explore trusted fetal monitoring options by Radiation Detection Company
Radiation Detection Company (RDC) is proud to offer various fetal monitoring solutions that meet our customers’ needs for accurate and reliable radiation dose measurements. Pregnant employees can trust in our solutions and choose from TLD, OSL, or NetDose™ digital dosimeter.
Learn more about fetal dosimetry solutions →



